BY Tim Dutton, UNITE Pinellas & Carl R. Lavender, Jr., Foundation for a Healthy St. Petersburg
ST. PETERSBURG — The rates of COVID-19 infection in Pinellas County are very different if you are black than if you are white, and the gap is widening quickly. It is a crisis, and WHAT is being done about it? What can be done about it?
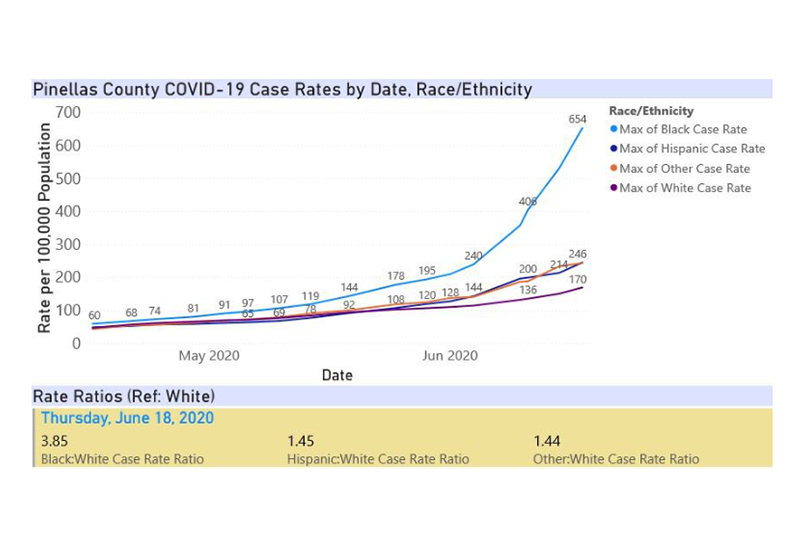
The racial disparity data for Pinellas County paints a bleak picture: Blacks are 3.85 times (2.37 times in Hillsborough County), more likely to be COVID-19 positive than whites. American Indian, Asian, Alaska Native, Hawaiian Islanders, collectively referred to as “Other” in state data, are 1.44 times more likely to be COVID-19 positive than whites in Pinellas (7 times more likely in Hillsborough County).
Furthermore, black individuals are at greater risk of death if they contract COVID-19. That story bears out in the Florida data, with blacks dying at 1.42 times the rate of whites.
Even before the COVID-19 pandemic, people who are black suffered a disproportionate impact of health conditions related to structural inequities such as racial residential segregation, which inherently limits access to quality schools. Quality housing, healthcare, and equal employment opportunities that structures access to health insurance, adequate income, wealth generation and paid time off are significant factors.
Arline Geronimus, University of Michigan researcher, concludes that “weathering” is a physical consequence of social inequality, which results from the deterioration of the body’s cells due to repeated adaptation to environmental and acute stressors. Add to the picture now COVID-19. Weathering has likely decreased the body’s ability to fight this virulent infection.
This phenomenon is well-known and inspired some communities and states to act quickly and decisively, anticipating the inevitable disproportionate outcomes. In April, the mayor of Chicago established a Racial Equity Rapid Response Team organized around the “pillars of Education, Prevention, Testing & Treatment, and Supportive Services.
This team was designed to “mount a public health response that addresses the specific and contextualized needs of our residents and families.”
In some cases, states identified the disproportionality and developed responses. In Maryland, Michigan, Mississippi, New York, South Carolina, and Virginia, neighborhoods that are predominately black are targeted for additional testing and contact tracing. States are distributing personal protective equipment, such as masks and hand sanitizers, door to door in hard-hit, predominately black communities.
In late March, even before most states were tracking race-related data about COVID-19, the Mayor of Shreveport created a digital map that anticipated the impact that the pandemic would have in the neighborhoods that are predominately black.
A June 3 article printed in the Washington Post says, “Advocates and public health researchers in Louisiana have said the lesson from cities such as Shreveport is to release race-related data more immediately and in more detail so local leaders have less guesswork about where to place resources.”
Hence, while much discussion has been generated across the country regarding the disproportionality of COVID cases and deaths by race, it has only moved some to action. There was no need to have waited to see the disparities in the data to be moved to action.
Now that the data are remarkably evident, specific strategies can and must be employed immediately, including:
- Aggressive targeted messaging to black community members that will be effective in educating about the need for PPE and testing
- Expand work with faith-based organizations, community organizations and trusted members of the black community to create and deliver messaging
- Purchase and distribute personal protective equipment (PPE) to blacks and others in communities experiencing high rates of COVID-19
- Advertise and encourage asymptomatic testing
- Hire additional persons to conduct testing and contact tracing
- Mobilize testing units to go door to door in black communities, and in other geographic areas where rates are higher
- Mobilize community health workers and navigators to provide education in their communities
- Provide full testing of the homeless population. Homeless individuals are also more susceptible to the effects of COVID-19, as they are more likely to suffer multiple comorbidities. They are also less likely to have no regular source of care, placing a greater burden on hospitals and public resources if they contract COVID-19
- Financial assistance should be provided when there is a confirmed case of COVID with economic impacts on an individual or family
It is now past the time for anticipation, and it is now the time for action.